Many of our survey participants expressed interest in learning more about dysphagia and ways to support their family member with dementia who may be dealing with dysphagia now or in the future. Here we are sharing the short answers to some common questions about dysphagia and dementia and where to go to learn more.
What is dysphagia?
Dysphagia is the medical term for swallowing difficulty. It is categorized according to where along the way the difficulties arise. For example, oral dysphagia refers to issues moving the food/liquid within the mouth, oropharyngeal dysphagia refers to issues moving the food/liquid into the back of the throat or pharynx, and esophageal dysphagia refers to issues moving the food/liquid down the esophagus to the stomach. Licensed medical professionals known as speech-language pathologists or speech therapists are specially trained to assess and treat swallowing disorders.
What causes dysphagia for someone with dementia?
Dysphagia can be caused by changes that occur in the brain as well as environmental factors, such as background noise, distractions, etc. While dysphagia tends to be more apparent in the later stages of dementia, it may be present to one degree or another at any stage of dementia.
What are signs that someone with dementia has dysphagia?
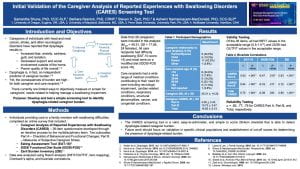
Potential signs or symptoms may include difficulty chewing, food left in the mouth, coughing during eating/drinking, reduced intake, taking longer to eat, avoiding certain foods, and weight loss. This brief questionnaire can help identify a possible swallowing disorder.
What are the risks of dysphagia?
Perhaps the most well-known risk is choking, which happens when food goes “down the wrong pipe” and obstructs breathing. Making a vocal sound like coughing is a good indicator that a person is not choking since airflow is needed for making sounds like coughing, talking, etc. Refer to the American Red Cross website for more information on how to recognize and respond to a choking event.
Lesser-known risks associated with dysphagia include malnutrition and dehydration as well as a serious condition called aspiration pneumonia, when aspirated material (i.e., food/liquid that enters the airway) becomes infected in the lungs.
How can I prevent aspiration pneumonia?
Routine oral care limits the bacterial load in the mouth and, therefore, limits the bacteria in any consumed food/liquid that may take a wrong turn and enter the lungs. So, proper oral hygiene is one way to help prevent this type of pneumonia.
Another way is to try to prevent aspiration (material entering the airway) in the first place. If you are noticing signs and symptoms of dysphagia, talk to your doctor about seeing a speech-language pathologist who can assess and come up with an individualized treatment plan. Part of the plan may include mealtime modifications, such as head posturing. Such modifications can be more effective at preventing aspiration and aspiration pneumonia than thickened liquids, a dietary modification that is also associated with an increased risk for dehydration. While feeding tubes are an option, research suggests that they do not prevent aspiration/aspiration pneumonia (what is being fed through the tube can come up and enter the airway), nor do they prolong life.
How do I help someone with dementia get the nutrition they need?
Maximizing sensory cues associated with eating (e.g., flavors, temperatures, textures) can improve meal engagement and nutritional intake among individuals with dementia. People with dementia may also prefer to eat multiple small meals and/or “finger foods” that can easily be eaten using hands instead of utensils. Setting up meals to suit these preferences, and any others you’ve identified, such as softer foods, familiar foods, etc., can lead to greater intake throughout the day.
To learn more about dysphagia and access dysphagia-related caregiver resources, visit the National Foundation of Swallowing Disorder website.